Spontaneous rupture of a giant hepatic hemangioma, case report and literature review .2
Picture 2. (a) Enhanced abdominal CT. Hemangioma in right liver lobe. Perihepatic pack (asterisk) (b) Involvement of segments 7 and 8. Bilateral pleural effusion (arrows).
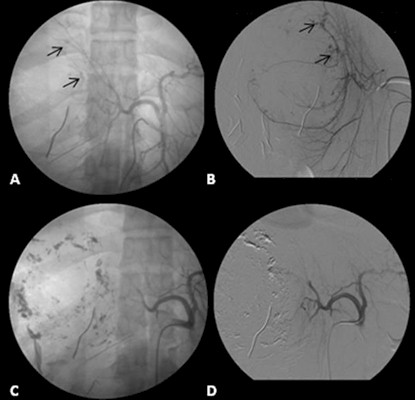
Picture 3. (A) Celiac angiogram and (B) Selective angiogram of right hepatic artery showing contrast extravasation. (Arrows) (C) Immediate embolization and (D) postembolization angiogram with absent arterial flow of the lesion

Picture 4. Postoperatory recovery
Discussion
Hemangioma is the most common bening tumor affecting the liver. It has a reported incidence rate at necropsy as high as 7%. (1,2,3) Hemangiomas are composed of masses of blood vessels that are atypical or irregular in arrangement and size. Most of hemangiomas are small, asymptomatic and detected by chance whereas larger and multiple lesions may produce symptoms. (4)
Women between 30 and 50 years old are more often affected than men, with a ratio of 5:1. (2,3,4,5) Some hemangiomas can increase during pregnancy and with estrogen medication. They are usually solitary lessions, although in some reports they have been identified as multiple lesions up to 50% of cases. They are more common in the right lobe of the liver. The most common size of these lesions range from 3 to 5 cm and when their size is bigger than 5 cm they are known as giant hemangiomas. Goodman noted that symptoms are experienced by 40% of patients with 4-cm hemangiomas and by 90% of patients with 10-cm hemangiomas. The most common symptoms are pain in the right upper quadrant (54%), nausea, vomiting, signs of extrinsic intestinal compression and hepatomegaly. (1,2,4,5,6)
Some long follow-up studies revealed absence of elongation in 80% of patients merely managed with observation. Spontaneous rupture is an extremely unusual presentation (1-4%) with a high mortality rate. (3,4,7) Until date there are only 32 published cases of spontaneous rupture in adults with only 5 survivors (33, Saudi)
Some authors have associated the giant hepatic hemangioma with thrombocytopenia, compsumption coagulopathy and microangiopathy (Kasabach-Merrit syndrome). (1)
Diagnosis can be radiological using methods like US, CT and MRI. Dynamic contrast-enhanced CT scanning is preferred, showing a low density mass with a marginal stain after injection of intravenous contrast. MRI is highly sensitive and specific, typically showing low signal intensity on T1-weighted images and high intensity on T2. MRI is very useful for small lesions (smaller than 2 cm). (4) Ultrasonography may show a roughly hypoechoic formation compared to the surrounding parenchyma although their sonographic appearance is variable and nonspecific.
Asymptomatic hemangiomas do not require treatment because of the low complication rates. However, some surgeons advocate resection of large (>10 cm) asymptomatic lesions because of the potential risk of spontaneous rupture. The size and location of a lesion will influence the surgeon’s decision to perform either a formal segmental resection of the hemangioma or an enucleation. Hepatic transplantation is indicated to symptomatic patients with surgically inoperable lesions or in case of a giant hemangioma with hemangiomatosis and associated Kasabach-Merrit syndrome. In some cases the efficiency of trascateter arterial embolization has been proved with fast recovery of the comsumption coagulopathy. (1,4,6,8,9,10)
In this case, the perihepatic packing done prior to referral may have contributed to stabilization. New exploratory laparotomy was obligated due to severe hipovolemic shock in order to reduce bleeding. Hepatic arterial embolization was made after hemodynamic stabilization achieving a good outcome.
Conclusion
The satisfactory evolution of this patient was due to the correct handle in the right time, patient’s age and the multidisciplinary handle in a third level hospital
References
1. Valdes Mas M, Ortiz Sánchez ML, Rodrigo Agudo JL, Miras López M, Pons Miñano JA, Carballo Alvarez F. Hemangioma hepático gigante asociado a síndrome de Kasabach-Merrit. Rev Esp Enf Dig 2008; 100: 511-513
2. Goodman Z. Benign tumors of the liver. In: Okuda K, Ishak KG. Neoplasms of the liver. Tokyo: Springer-Verlag; 1987:105-125.
3. Corigliano N, Mercantini P, Amodio PM, Balducci G, Caterino S, Ramacciato G, et al. Hemoperitoneum from a spontaneous rupture of a giant hemangioma of the liver: report of a case. Surg Today. 2003;33:459-63.
4. Dickie B, Dasgupta R, Nair R, Alonso MH, Ryckman FC, Tiao GM, et al. Spectrum of hepatic hemangiomas: management and outcome. J Pediatr Surg. 2009;44:125-33.
5. Glinkova V, Shevah O, Boaz M, Levine A, Shirin H. Hepatic hemangiomas: possible association with female sex hormones. Gut. 2004;53:1352-1355
6. Giannitrapani L, Soresi M, La Spada E, Cervello M, D’Alessandro N, Montalto G, Sex hormones and risk of liver tumor. Ann N Y Acad Sci. 2006; 1089: 228-236.
7. Cárcamo IC, López SJ, Tumores hepáticos benignos Cuad. Cir. 2006; 20: 79-85
8. Fernández Rodríguez V, Paz Martínez C, Gómez-Ulla AD, Graña Fernández S. Apuntes de ecografía. Hígado (III): Lesiones focales. Cad Aten Primaria Ano 2009; 16: 48-59
9. Benavides C, García C, Rubilar P, Covacevich S, Perales C, Ricarte F. Hemangiomas hepáticos. Rev. Chilena de Cirugía. 2006; 58: 194-198
10. Macías Robles MD, Martínez Mengual BM, Rodríguez Rodríguez MI, Amador Tejón MJ. Hemangioma hepático cavernoso gigante. Emergencias 2009; 21: 232
11. Lloret P. Tratamiento médico de los hemangiomas. An Sist Sanit Navar 2004; 27: 81-92.
12. Vassiou K, Rountas H, Liakou P, D. Arvantis D, Fezoulidis I, Tepetes K, Embolization of a Giant Hepatic Hemangioma Prior To Urgent Liver Resection. Case Report and review of the Literature. Cardiovasc Intervent Radiol. 2007; 30: 800-802
13. Jain V, Ramachandran V, Garg R, Pal S, Gamanagatti SR, Srivastava DN, Spontaneous rupture of a giant hepatic hemangioma - sequential management with transcatheter arterial embolization and resection. Saudi J Gastroenterol. 2010; 16:116-119
14. Koike N, Cho A, Nasu K, Seto K, Nagaya S, Ohshima Y, et al. Role of diffusion-weighted magnetic resonance imaging in the differential diagnosis of focal hepatic lesions. Worl J Gastroenterol 2009;15: 5805-5812
15. Brogna A, Ferrara R, Bucceri AM, Virgilio C, Scalisi G, An atypical case of hepatic cavernous hemangioma. Cases Journal 2009; 2: 181
16. Boiulac-Sage P, Laumonier H, Laurent C, Blanc JF, Balabaud C, Benign and Malignant Vascular Tumors of the Liver in Adults. Semin Liver Dis. 2008; 28: 302-314